Background
Systemic mastocytosis (SM) is a rare, clonal mast cell disease driven by the KIT D816Vmutation in ~95% of cases and can be subdivided into two predominant subtypes - advanced SM (AdvSM) and indolent SM (ISM). AdvSM comprises ~15% of all patients and is characterized by mast cell proliferation and infiltration causing subsequent dysfunction of various organ systems, leading to reduced overall survival. Indolent systemic mastocytosis (ISM) comprises the bulk of the remaining ~85% of patients and is characterized by a less severe clinical course that is nevertheless associated with a significant symptom burden that may worsen over time, poor quality of life, and the potential for life-threatening anaphylaxis. Recent epidemiologic data indicate ISM is a heterogenous disease. A meaningful subset of patients with disease risk factors demonstrates high symptom burden, which may be associated with higher rates of disease progression and increased risk of death (Sperr, et al. Lancet Hematol. 2019). Building upon this work, we conducted an analysis to evaluate overall survival (OS) in ISM patients.
Methods
Using a nationally representative health claims dataset provided by Komodo Health covering 230 million US patients (2015 to 2022), we identified 8,332 patients with ISM using a claims-based algorithm. This algorithm leverages combinations of ICD-10 dx codes for SM and organ dysfunction, procedure codes (bone marrow biopsy), and use of SM-directed therapies (Mukherjee et al ASH 2022). Patients were included if full medical and pharmacy claim information was available for >12 consecutive months post-diagnosis, and median follow-up was 4.0 years. ISM was inferred as a dx if only the broad systemic mastocytosis ICD-10 code was used (D47.02) and there was no preceding evidence of AdvSM or an associated hematologic neoplasm. Disease progression to AdvSM was inferred if there was subsequent evidence of mast cell leukemia, aggressive SM, or an associated hematologic neoplasm OS was then calculated, anchored to the first observed ICD-10 dx code for SM. Mortality information was available within the claims dataset and was additionally inferred if a patient did not generate any medical or pharmacy claims for 12 or more consecutive months.
Three, independent non-SM control cohorts (N=2000 each) were established for comparison, based on a stratified sampling strategy matched by gender, age, Charlson Comorbidity Index, payer status, and race/ethnicity of the ISM population. Multiple cohorts were plotted to illustrate consistency in survival across independently-sampled control cohorts. As positive control, we compared OS with a cohort of patients with ASM, a disease cohort with known increased mortality.
Results
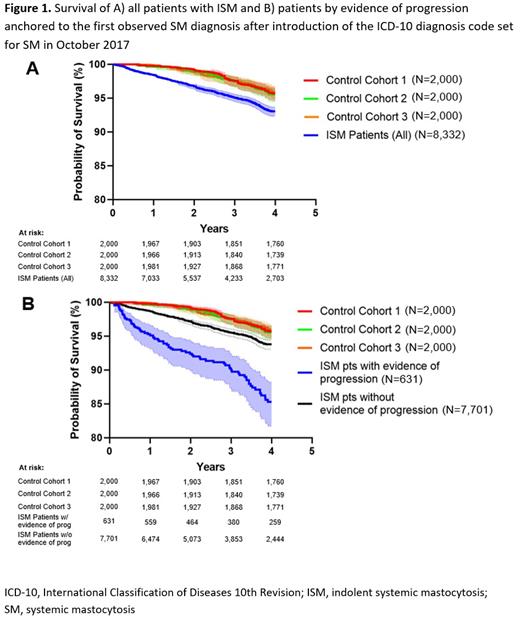
We observed a statistically significant difference in OS among patients with ISM versus the matched non-SM control cohorts ( p<0.0001, with a log-rank hazard ratio of 1.64; Figure 1A). Excess mortality was noted among ISM patients with or without evidence of disease progression ( p<0.0001, with a hazard ratio of 1.44) compared to matched non-SM cohorts ( Figure 1B). As expected, OS was worst in patients with AdvSM ( p<0.0001, with a hazard ratio of 6.64).
The ISM cohort presented to the emergency room (ER) 0.70 times per year, compared to 0.31 times per year for the combined non-ISM control cohorts, based on the sum of ER visits observed across the cumulative cohort observation period. Patients with ISM who died during the study interval had the highest frequency of ER visits, at a rate of 1.09 visits per year.
Conclusions
This is the first and the largest population-level analysis of OS in the ISM population in the US. Results demonstrate a modest but statistically significant decrease in survival among these patients even early in their disease course (first 4 years). This increase in mortality was observed even among patients with no evidence of progression to advanced SM and was additionally associated with >2x higher rates of ER visits over the observation period. These results suggest that acute, severe symptoms of SM may contribute to the excess mortality seen among patients with ISM and warrant focused research to identify specific patient characteristics or disease features in ISM that confer higher risk of mortality.
Disclosures
Mukherjee:Celgene/Acceleron: Other: Advisory Board; Genentech and AbbVie: Other: Advisory Board; Bristol Myers Squibb: Other: Advisory Board; Novartis: Other: Advisory Board; Blueprint Medicines Corporation: Other: Advisory Board; BioPharm: Consultancy; EUSA: Honoraria; McGraw Hill Hematology Oncology Board Review: Honoraria; Bristol Myers Squibb: Honoraria; Celgene (now BMS): Honoraria; Aplastic Anemia and MDS International Foundation: Honoraria; EUSA: Other: Advisory Board; Celgene (now BMS): Research Funding; Novartis: Consultancy; Celgene (now BMS): Consultancy; Bristol Myers Squibb: Consultancy; Novartis: Research Funding; Jazz Pharmaceuticals: Research Funding. Cattie:Blueprint Medicines Corporation: Current Employment, Current equity holder in publicly-traded company. Shaheen:Blueprint Medicines Corporation: Current Employment, Current equity holder in publicly-traded company. Powell:Blueprint Medicines Corporation: Current Employment, Current equity holder in publicly-traded company. Green:Blueprint Medicines Corporation: Current Employment, Current equity holder in publicly-traded company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal